Mould infections
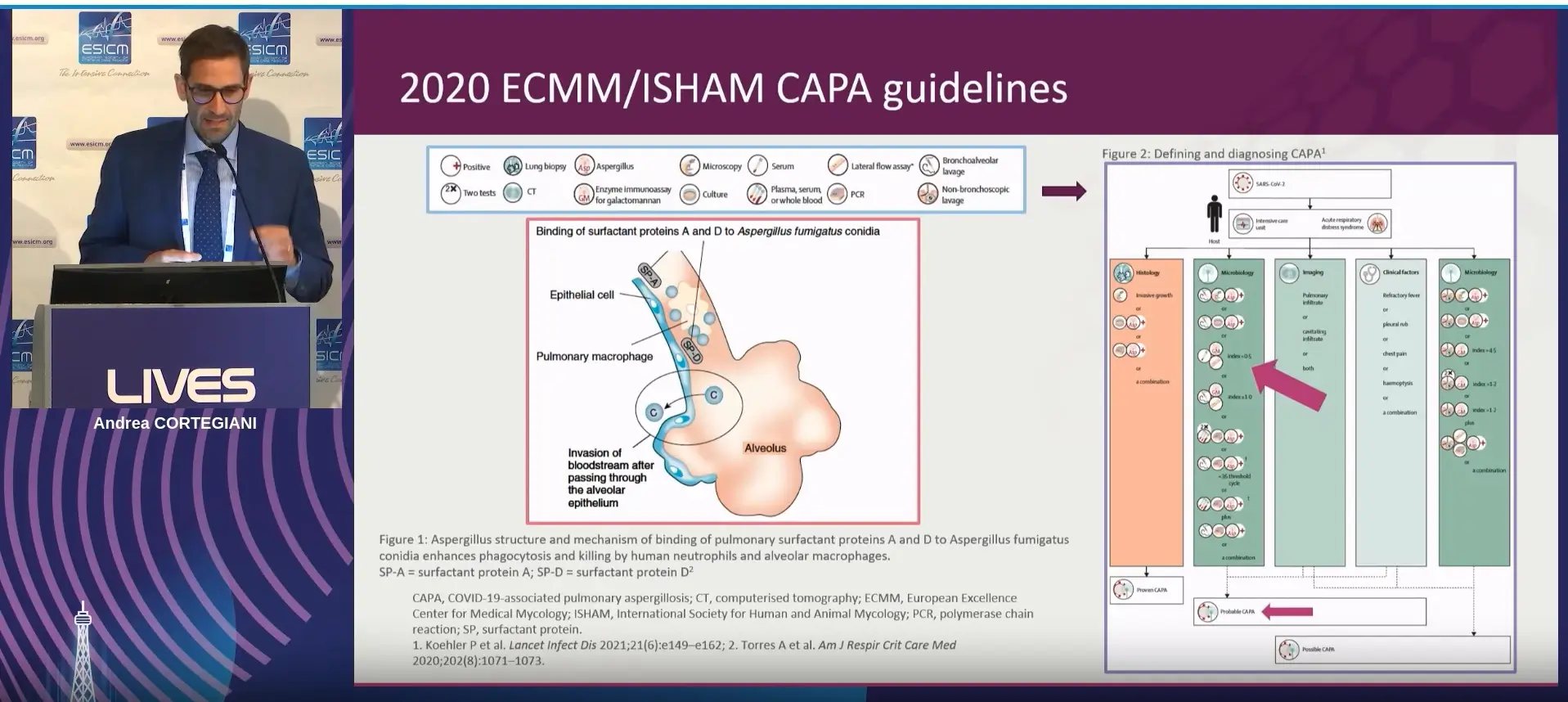
Invasive aspergillosis (IA)
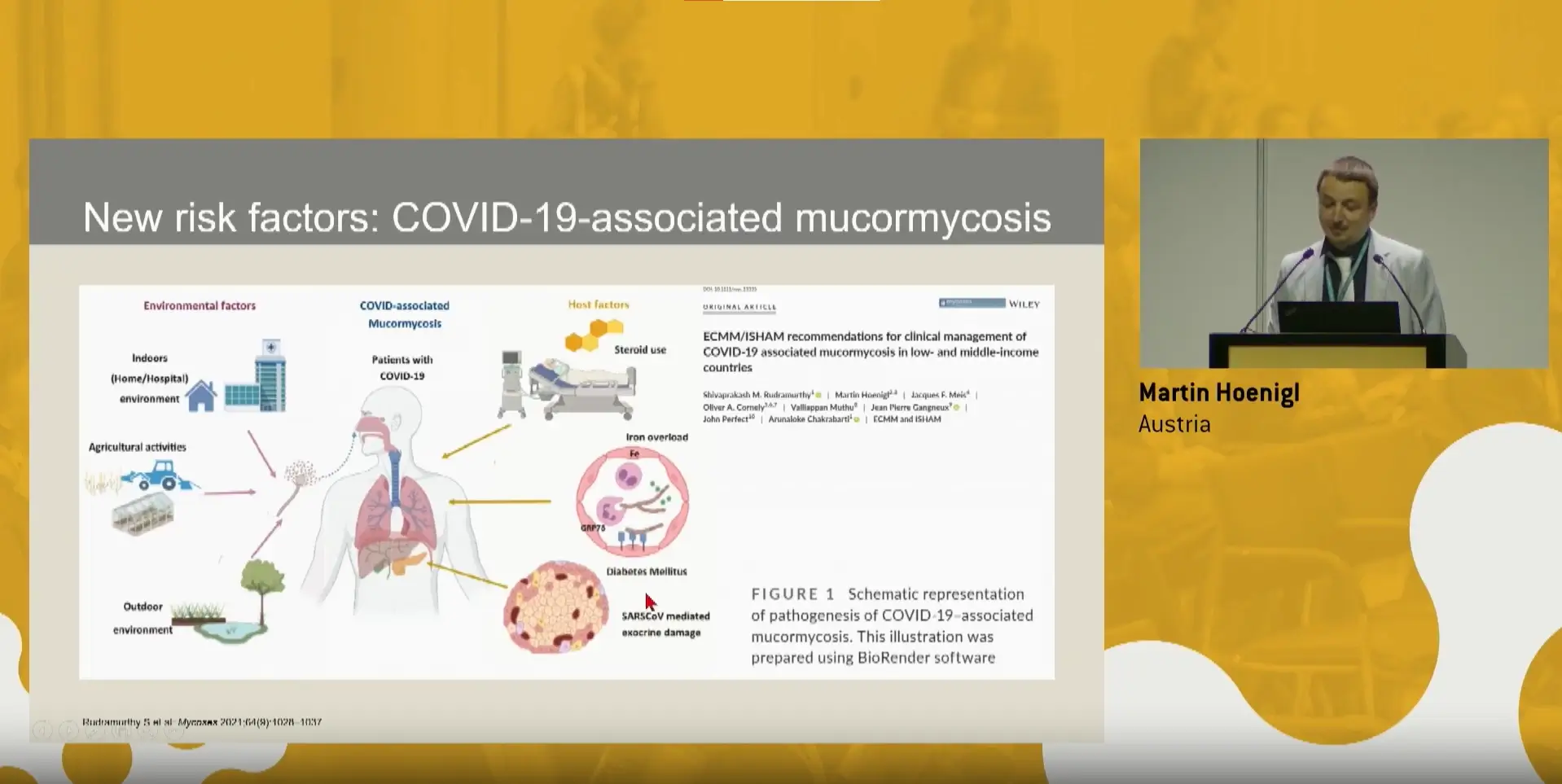
Mucormycosis
Rare mould infections
Eumycetoma
Fusariosis
Lomentosporiosis
Scedosporiosis
Dimorphic fungal infections
Coccidiomycosis
Histoplasmosis
Paracoccidioidomycosis
Talaromycosis
Yeast infections
Cryptococcosis
Invasive candidiasis (IC)
Yeast-like infections
Pneumocystis pneumonia (PJP)
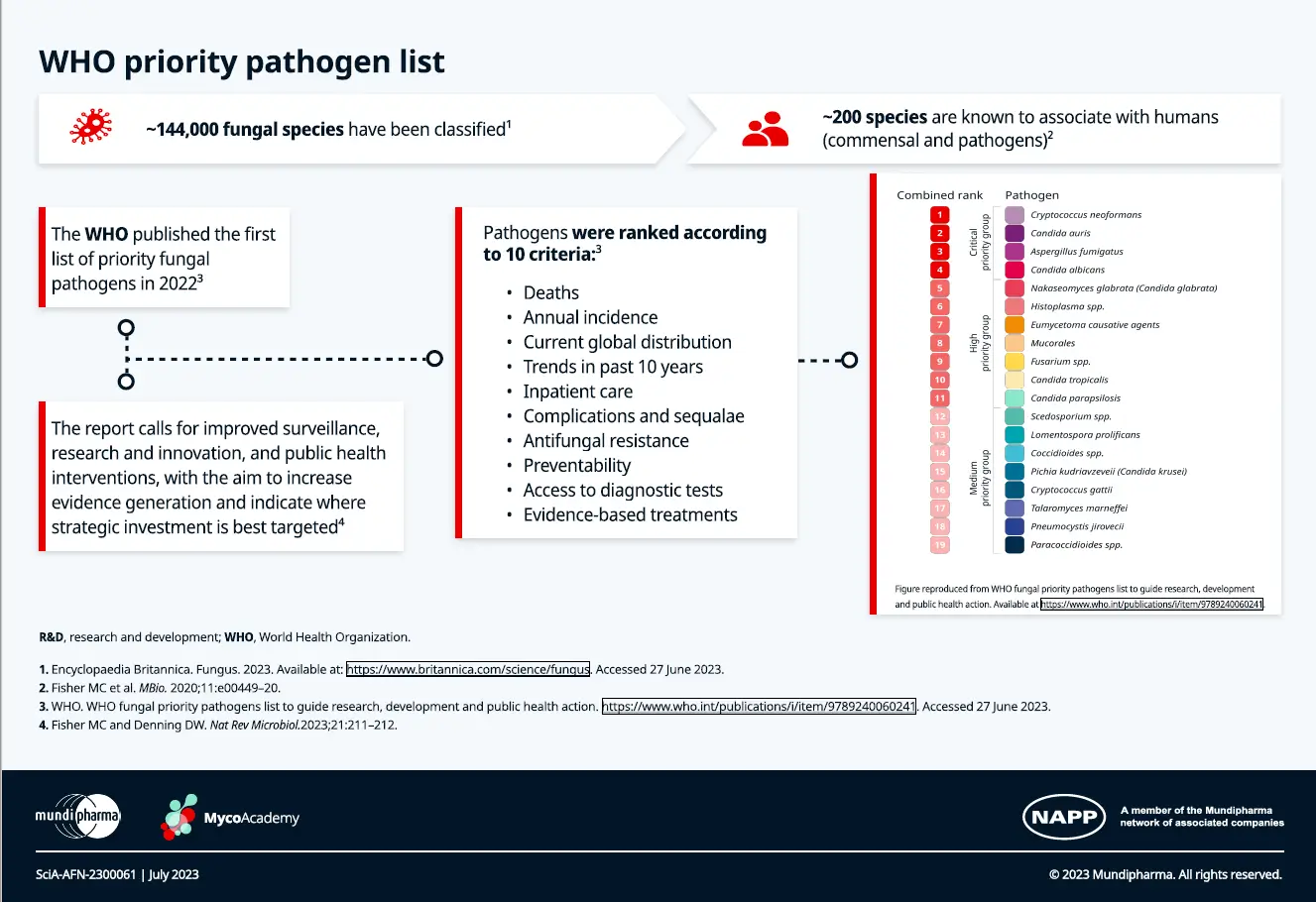
The burden of fungal infections
Invasive fungal infections are a major global health concern. Serious fungal infections affect more than 150 million people worldwide, and are responsible for over 1.6 million deaths per year.7,8
IFDs are an important cause of morbidity and mortality, particularly in patients with altered immune function, and overall cases have been rising.8
Coronavirus disease 2019 (COVID-19) has been associated with an increase in the incidence of comorbid IFDs such as aspergillosis, mucormycosis and candidemia, often with harmful consequences.8
Precise estimates of global prevalence and incidence of each fungal infection remain unknown; data are insufficient in some countries, especially those in low-to-middle income countries.7
Knowledge on the global incidence of fungal diseases has been impaired by a lack of regular national surveillance systems, no obligatory reporting of cases of fungal diseases, poor clinician investigation outside of specialised units, poor diagnostic test performance and few well-designed published studies.7
Global burden and annual incidence of fungal diseases
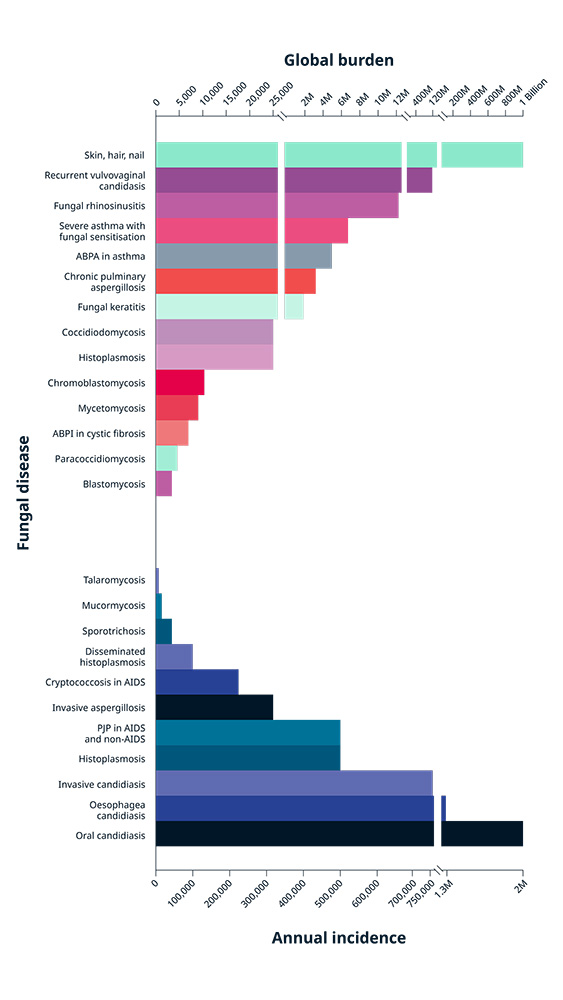
Figure adapted from Bongomin F et al. J Fungi (Basel) 2017.
ABPA, allergic bronchopulmonary aspergillosis; AIDS, acquired immunodeficiency syndrome;
PJP, Pneumocystis pneumonia.
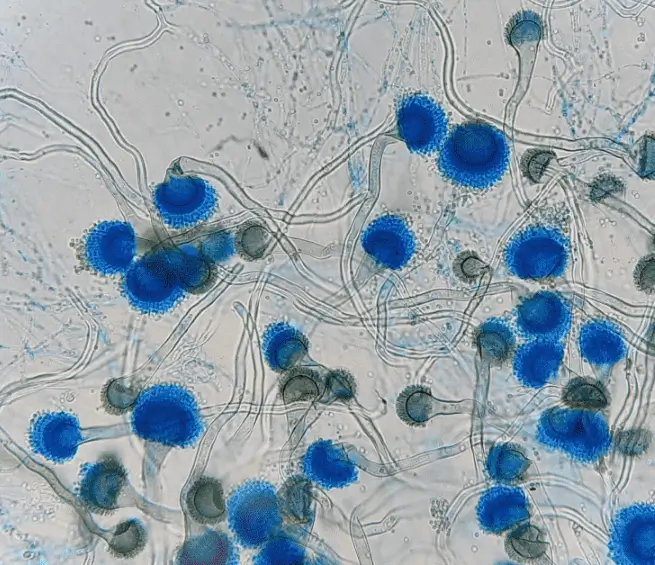
Aspergillus fumigatus
30–95%
Candida albicans
46–75%
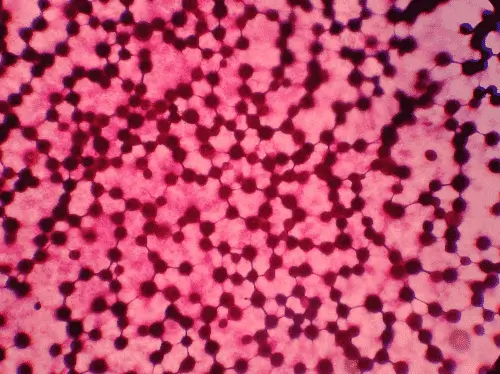
Cryptococcus neoformans
20–70%
Pneumocystis jirovecii
20–80%

There are different antifungal treatment strategies to help manage invasive fungal infections. Notably, there are four antifungal classes available to treat invasive fungal infections, including azoles, polyenes, echinocandins and pyrimidine analogues.11
At MycoAcademy, healthcare professionals (HCPs) are equipped with comprehensive, evidence-based educational resources on invasive fungal infections. These materials, developed in collaboration with leading experts in the field, are designed to support experienced HCPs seeking to deepen their knowledge, as well as those early in their careers who are embarking on their journey within this critical area of healthcare.
Educational resources
Latest hot topics
Case studies
References
- Fang W, Wu J, Cheng M, Zhu X, Du M, Chen C, et al. Diagnosis of invasive fungal infections: challenges and recent developments. J Biomed Sci. 2023 Jun 19;30(1):42.
- Walsh TJ, Dixon DM. Spectrum of mycoses. In: Medical Microbiology. Galveston (TX): University of Texas Medical Branch at Galveston; 1996.
- Delaloye J, Calandra T. Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence. 2014 Jan 1;5(1):161–9.
- Antachopoulos C, Walsh TJ, Roilides E. Fungal infections in primary immunodeficiencies. Eur J Pediatr. 2007 Nov;166(11):1099–117.
- Köhler JR, Casadevall A, Perfect J. The spectrum of fungi that infects humans. Cold Spring Harb Perspect Med. 2014 Nov 3;5(1):a019273.
- King J, Pana ZD, Lehrnbecher T, Steinbach WJ, Warris A. Recognition and clinical presentation of invasive fungal disease in neonates and children. J Pediatric Infect Dis Soc. 2017 Sep 1;6(suppl_1):S12–21.
- Bongomin F, Gago S, Oladele RO, Denning DW. Global and multi-national prevalence of fungal diseases-estimate precision. J Fungi (Basel). 2017 Oct 18;3(4):57.
- World Health Organization. WHO fungal priority pathogens list to guide research, development and public health action. Genève, Switzerland: World Health Organization; 2022. 48 p.
- Brown GD, Denning DW, Gow NAR, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012 Dec 19;4(165):165rv13.
- Sarden N, Yipp BG. Virus-associated fungal infections and lost immune resistance. Trends Immunol. 2023 Apr;44(4):305–18.
- Azim A, Ahmed A. Diagnosis and management of invasive fungal diseases in non-neutropenic ICU patients, with focus on candidiasis and aspergillosis: a comprehensive review. Front Cell Infect Microbiol. 2024 Mar 5;14:1256158.