Antifungal classes
The four main antifungal classes available for the treatment of IFDs are:1
Azoles1,2
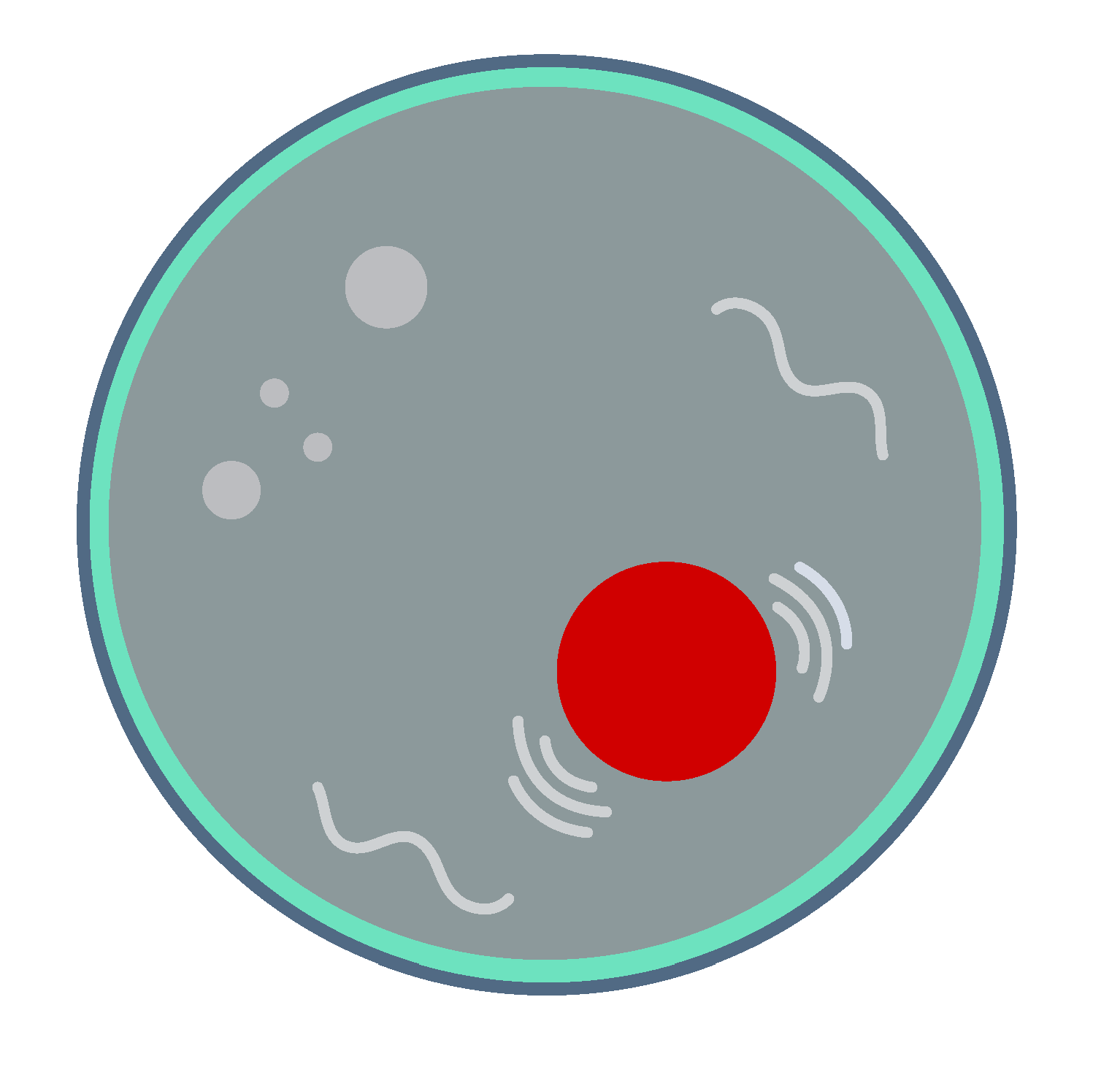
Disrupt sterol synthesis by inhibiting cytochrome P450 (CYP)-dependent C-14α demethylase, a crucial fungal CYP enzyme involved in the conversion of lanosterol to ergosterol in the cell membrane, leading to cell damage.
Polyenes2
Destabilise the fungal cell membrane by binding to ergosterol, a key component of the fungal cell membrane. This binding results in the formation of pores in the membrane, causing depolarisation and subsequent leakage of the cell.
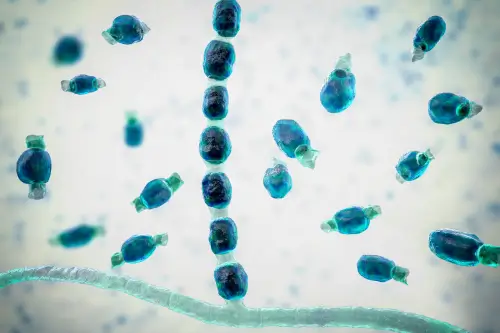
Echinocandins2
Inhibit β-1,3-glucan synthesis through the inhibition of β-1,3-glucan synthase (via Fks subunits). This results in heightened cell-wall permeability and the subsequent lysis of the fungal cell.
Pyrimidine analogues2
Convert to 5-fluorouridine triphosphate, which integrates into fungal RNA, disrupting protein synthesis. The intermediate 5-fluorocytosine inhibits thymidylate synthetase, interfering with DNA synthesis.
Treatment strategies
Antifungal treatment strategies can be classified as targeted or untargeted.1
Targeted
Targeted treatments are antifungal agents administered after definitive microbiological proof of infection.1
Untargeted
Untargeted treatments include the use of an antifungal agent prior to definitive microbiological diagnosis.1
There are four possible strategies used in the treatment of IFDs:
Prophylactic treatment
Administered to patients at high risk of IFDs without apparent symptoms to prevent fungal infection.1–4
Empirical treatment
Administered to patients with high-risk conditions displaying established clinical symptoms of IFD without a known cause and lacking microbiological evidence.1,4–7
Pre-emptive treatment
Uses non-culture-based microbiological evidence, such as rapid diagnostic tests to direct therapy in patients at risk of IFD development.1,2,4
Targeted treatment
Administered after definitive microbiological confirmation and confirmatory tests.1
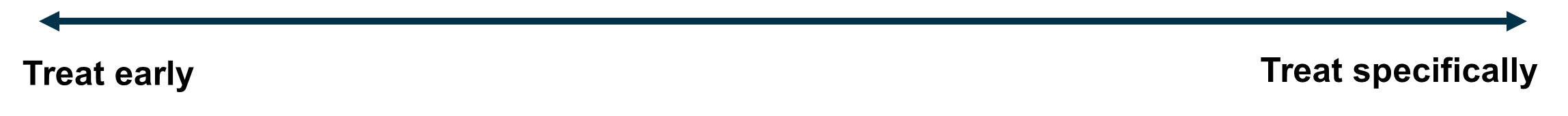
Management strategies should follow a patient-centred approach based on the risk-group of the patient and their unique clinical situation8
Prophylactic treatment:
Empirical treatment:
Pre-emptive treatment:
Targeted treatment:
*Risk factors may include patients presenting with persistent and refractory fever, critically ill patients in the ICU, limited response to broad-spectrum antibiotics, severe sepsis and neutropenia after haematopoietic stem cell transplantation.
Antifungal stewardship (AFS)
AFS refers to interventions to monitor and direct the right use of antifungal agents.1
Treatment guidelines
European and international bodies have published guidelines on IFD treatment across different patient subgroups. Select the type of IFD to access the relevant treatment guideline. Last updated: April 2024.
Yeast and yeast-like infections
Dimorphic fungal infections:
References
Antifungal classes
- Johnson MD. Infect Dis Clin North Am. 2021;35:341–371.
- Gubbins PO, Anaissie EJ. Chapter 7: Antifungal therapy. In: Anaissie EJ, et al. (eds). Clinical Mycology (second edition). Churchill Livingstone: Elsevier Inc, 2009.
Treatment strategies
- Cortegiani A et al. Cochrane Database Syst Rev. 2016;2016:CD004920.
- Gangneux JP et al. Infect Dis Ther. 2018;7(3):309–325.
- Robenshtok E et al. J Clin Oncol. 2007;25(34)5471–5489.
- Bassetti M et al. Critical Care. 2010;14:244.
- Zaragoza R et al. Ther Clin Risk Manag. 2008;4(6):1261–1280.
- Bretonnière C et al. J Thorac Dis. 2016;8(12):E1719–E1722.
- Pagano L et al. Haematologica. 2011;96(9):1366–1370.
- WHO. WHO fungal priority pathogens list to guide research, development and public health action. https://www.who.int/publications/i/item/9789240060241. Accessed April 2024.
AFS
- Khanina A et al. Int Med Journal. 2021;51:18‒36.
- Johnson MD et al. J Infect Dis. 2020;222:S175‒S198.
- Chakrabarti A et al. Open Forum Infect Dis. 2022;9:ofac234.
- Perlin DS et al. Lancet Infect Dis. 2017;17:e383–e392.
- Talento AF et al. J Fungi (Basel). 2021;7:801.
SciA-AFN-2400025 | April 2024